Une équipe internationale dirigée par les universités de Bristol, au Royaume-Uni, et d’Auckland, en Nouvelle-Zélande, a enfin résolu l’énigme qui se posait depuis longtemps, à savoir pourquoi tant de patients souffrant d’une pression artérielle élevée (connue sous le nom d’hypertension) sont également atteints de diabète (glycémie élevée).
Cette nouvelle découverte importante a montré qu’une petite protéine, le glucagon-like peptide-1 (GLP-1), couple le contrôle de la glycémie par l’organisme. et la pression artérielle.
Le professeur Julian Paton, auteur principal, et directeur de Manaaki Mãnawa – The Centre for Heart Research à l’université d’Auckland, a déclaré : “Nous savons depuis longtemps que l’hypertension et le diabète sont inextricablement liés et nous avons enfin découvert la raison, qui va maintenant informer de nouvelles stratégies de traitement.”
La recherche, publiée en ligne avant impression dans Circulation Research le 1er février 2022, a impliqué des contributions de scientifiques collaborant au Brésil, en Allemagne, en Lituanie et en Serbie, ainsi qu’au Royaume-Uni et en Nouvelle-Zélande.
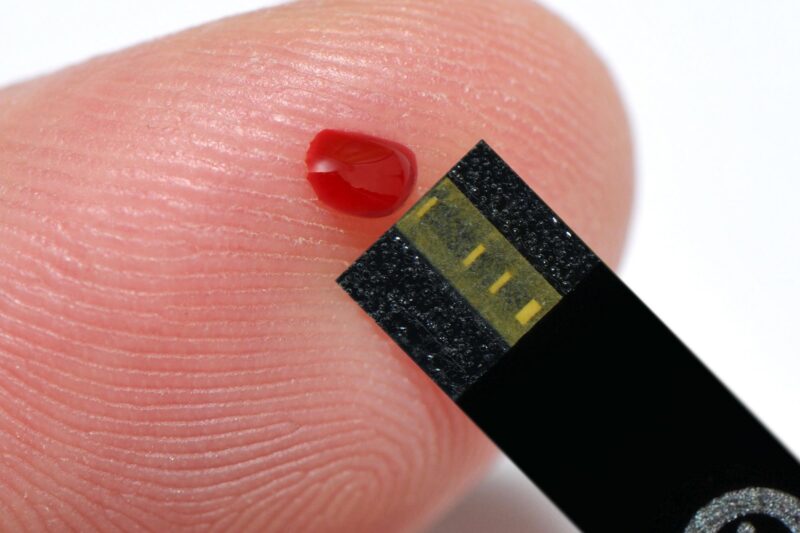
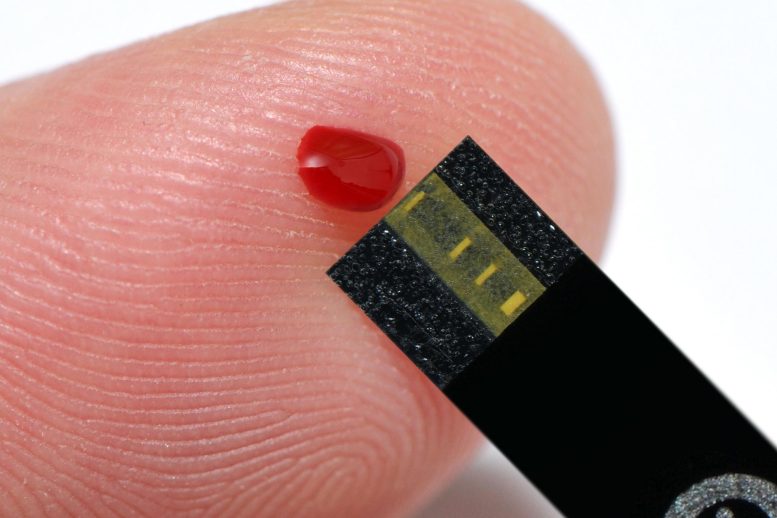
Le GLP-1 est libéré par la paroi de l’intestin après un repas et agit pour stimuler l’insuline du pancréas afin de contrôler la glycémie. On le savait déjà, mais on a découvert que le GLP-1 stimule également un petit organe sensoriel appelé corps carotidien, situé dans le cou.
L’University of Bristol group used an unbiased, high-throughput genomics technique called RNA sequencing to read all the messages of the expressed genes in the carotid body in rats with and without high blood pressure. This led to the finding that the receptor that senses GLP-1 is located in the carotid body, but less so in hypertensive rats.
David Murphy, Professor of Experimental Medicine from Bristol Medical School: Translational Health Sciences (THS) and senior author, explained: “Locating the link required genetic profiling and multiple steps of validation. We never expected to see GLP-1 come up on the radar, so this is very exciting and opens many new opportunities.”
Professor Paton added: “The carotid body is the convergent point where GLP-1 acts to control both blood sugar and blood pressure simultaneously; this is coordinated by the nervous system which is instructed by the carotid body.”
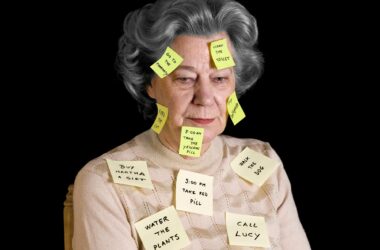
People with hypertension and/or diabetes are at high risk of life-threatening cardiovascular disease. Even when receiving medication, a large number of patients will remain at high risk. This is because most medications only treat symptoms and not causes of high blood pressure and high sugar.
Professor Rod Jackson, world-renowned epidemiologist from the University of Auckland, said “We’ve known that blood pressure is notoriously difficult to control in patients with high blood sugar, so these findings are really important because by giving GLP-1 we might be able to reduce both sugar and pressure together, and these two factors are major contributors to cardiovascular risk.”
Mr. Audrys Pauža, a British Heart Foundation-funded PhD student in Professor David Murphy’s lab in the Bristol Medical School and lead author on the study, added: “The prevalence of diabetes and hypertension is increasing throughout the world, and there is an urgent need to address this.
“Drugs targeting the GLP-1 receptor are already approved for use in humans and widely used to treat diabetes. Besides helping to lower blood sugar these drugs also reduce blood pressure, however, the mechanism of this effect wasn’t well understood.
“This research revealed that these drugs may actually work on the carotid bodies to enact their anti-hypertensive effect. Leading from this work, we are already planning translational studies in humans to bring this discover into practice so that patients most at risk can receive the best treatment available.”
But GLP-1 is just the start. The research has revealed many novel targets for ongoing functional studies that the team anticipate will lead to future translational projects in human hypertensive and diabetic patients.
Reference: “GLP1R Attenuates Sympathetic Response to High Glucose via Carotid Body Inhibition” by Audrys G. Pauza, Pratik Thakkar, Tatjana Tasic, Igor Felippe, Paul Bishop, Michael P. Greenwood, Kristina Rysevaite-Kyguoliene, Julia Ast, Johannes Broichhagen, David J. Hodson, Helio C. Salgado, Dainius H. Pauza, Nina Japundzic-Zigon, Julian F.R. Paton and David Murphy, 1 February 2022, Circulation Research.
DOI: 10.1161/CIRCRESAHA.121.319874
The study was funded by the British Heart Foundation and the Health Research Council of New Zealand.