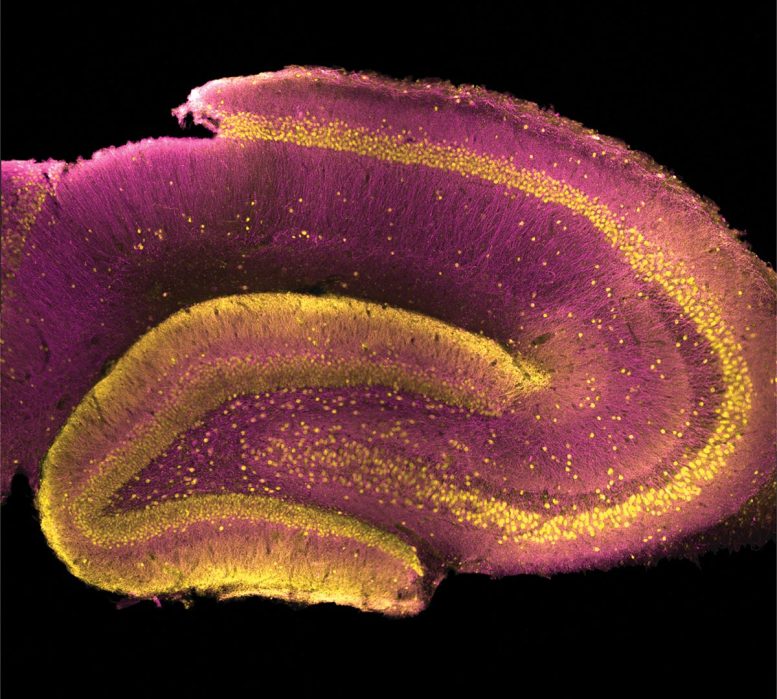
Le gyrus denté apparaît comme un corps épais, principalement jaune, en forme de C au centre gauche de cette coupe transversale de l’hippocampe d’un rat. Crédit : USC Dornsife/Yuni Kay
Des chercheurs qui étudient une protéine fortement liée à un trouble psychiatrique sont les premiers à déterminer la fonction de cette protéine, en la reliant à une structure de l’hippocampe appelée le gyrus denté.
En résolvant un mystère vieux de plusieurs décennies concernant une protéine particulière, les scientifiques ont identifié un endroit spécifique du cerveau où la schizophrénie pourrait trouver son origine.
Les nouvelles : Malgré l’identification de nombreux gènes ayant un lien avec la schizophrénie, il s’est avéré extrêmement difficile, jusqu’à présent, d’identifier avec un haut niveau de certitude une partie du cerveau susceptible d’être responsable de cette maladie.
Pourquoi c’est important : Savoir où chercher et ce qu’il faut chercher pourrait aider à identifier les personnes à risque de schizophrénie avant que la maladie ne se déclare et pourrait conduire à de nouvelles mesures de diagnostic, de prévention et de traitement.
- La schizophrénie touche environ 20 millions de personnes dans le monde.
- Les symptômes comprennent des hallucinations, des délires, un affect plat (manque d’expression émotionnelle), une perte du sens de l’identité personnelle et une perte de mémoire.
Une protéine sans rôle
L’étude, menée par des chercheurs du Fondée en 1880, la University of Southern California> ; est l’une des principales universités de recherche privées du monde. Elle est située au cœur de Los Angeles.
;” data-gt-translate-attributes=”[{” attribute=””>USC Dornsife College of Letters, Arts and Sciences and published online Feb. 10 in Nature Communications, centers on a protein centers on a protein called synapse-associated protein 97, or SAP97, that is found in neurons in the brain.
- Scientists have recently discovered that mutations inhibiting SAP97 function can give rise to schizophrenia.
- These mutations are linked to a 40-fold increase in the risk of developing schizophrenia — the largest increase in risk documented for any mutation to date.
- The normal function of SAP97 — that is, what it normally does and where it does it in the brain — has remained elusive for many years.
- Not knowing how or where the protein works has also kept a veil over why mutations in SAP97 would lead to schizophrenia.
From the principal researcher: “Reduced SAP97 function may very well give rise to the largest increase in schizophrenia risk in humans that we know of, but the function of SAP97 has been a total mystery for decades. Our study reveals where SAP97 functions in the brain and shows exactly what schizophrenia-associated mutations in this protein do to neurons.”
— Bruce Herring, assistant professor of biological sciences at USC Dornsife
A deeper look
SAP97 belongs to a family of proteins that regulate glutamatergic signaling between neurons and influence how memories are created and stored.
- Glutamatergic signaling is an important way neurons communicate with each other that involves neurons releasing the neurotransmitter glutamate onto neighboring neurons.
- Experiments up to now have failed to show that SAP97 plays any significant part in regulating glutamatergic signaling in the brain.
- The lack of evidence for SAP97 function in regulating communication between neurons has frustrated scientists, given the growing evidence of the protein’s connection to schizophrenia.
What they did: With no SAP97 activity apparent in traditionally studied brain regions, Herring and his team chose to look at a different region of the brain that has been theoretically linked to schizophrenia, called the dentate gyrus.
- The dentate gyrus is located within the hippocampus.
- It controls contextual episodic memory — the conscious recollection of life experiences that includes what happened along with when and where it happened.
- Contextual episodic memory is often altered in those with schizophrenia, and such alterations may contribute to the development of other symptoms associated with the disorder.
Studying rats with damaged SAP97, the researchers looked for changes in activity in the dentate gyrus — and they found them.
- Neurons in the dentate gyrus with reduced SAP97 function showed extremely large increases in glutamatergic signaling.
- The increase in signaling with mutated SAP97 suggests the protein normally helps dampen glutamatergic signaling specifically within the dentate gyrus.
- The large increases in glutamatergic signaling in the dentate gyrus caused by reduced SAP97 function also produced significant deficits in contextual episodic memory in rodents — a hallmark of schizophrenia.
A scientific first: The results are the first to confirm where in the brain SAP97 is active and to directly link alterations in dentate gyrus function to the development of schizophrenia.
What’s next?
In future studies, Herring and his team plan to look for SAP97 activity in other areas of the brain.
They will also determine whether schizophrenia-linked mutations in other proteins produce similar increases in glutamatergic signaling in the dentate gyrus.
Their ongoing work will significantly aid the development of more effective treatment strategies for this historically enigmatic disorder.
Reference: “Schizophrenia-associated SAP97 mutations increase glutamatergic synapse strength in the dentate gyrus and impair contextual episodic memory in rats” by Yuni Kay, Linda Tsan, Elizabeth A. Davis, Chen Tian, Léa Décarie-Spain, Anastasiia Sadybekov, Anna N. Pushkin, Vsevolod Katritch, Scott E. Kanoski and Bruce E. Herring, 10 February 2022, Nature Communications.
DOI: 10.1038/s41467-022-28430-5
In addition to corresponding author Herring, additional researchers on the study are USC Dornsife graduate students Yuni Kay (first author), Linda Tsan, Chen Tian and Anna Pushkin; USC Dornsife postdocs Léa Décarie-Spain and Anastasiia Sadybekov; Vsevolod Katritch, associate professor of quantitative and computational biology and chemistry, and Scott Kanoski, associate professor of biological sciences; and former USC Dornsife postdoc Elizabeth Davis.
The study was funded by National Institute of Mental Health grant number MH103398, National Institute of Neurological Disorders and Stroke grant number NS112480 and the Simons and McKnight Foundations.



