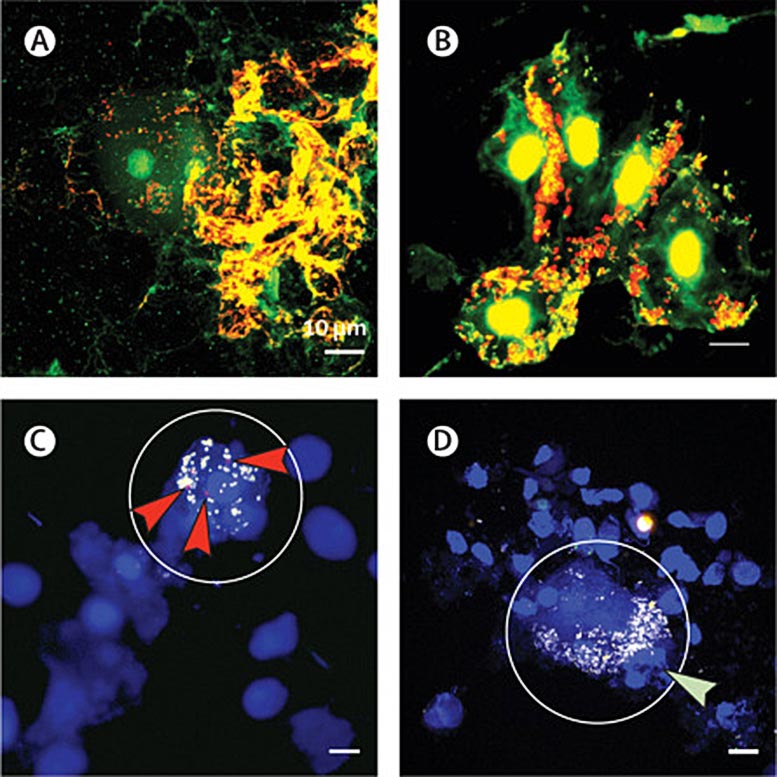
Biofilms de cellules épithéliales squameuses observés dans le lavage bronchoalvéolaire d’enfants souffrant de bronchite bactérienne prolongée ou de bronchectasie. Projections représentatives d’intensité maximale de lavage broncho-alvéolaire coloré avec BacLight (A-B), sondes d’hybridation in situ fluorescentes (FISH) (C-D), ou hématoxyline et éosine (E-F). Dans les images BacLight, l’ADN à l’intérieur des bactéries intactes (vivantes) est coloré en vert tandis que l’ADN extracellulaire et les bactéries perméables (mortes) sont colorés en rouge. (A) Lavage broncho-alvéolaire coloré au BacLight d’un enfant atteint de bronchite bactérienne prolongée (PBB) montrant de grands biofilms contenant des bactéries vivantes et mortes attachées aux cellules épithéliales squameuses. (B) Lavage broncho-alvéolaire coloré par BacLight d’un enfant atteint de bronchiectasie montrant des bactéries vivantes et mortes dans des biofilms attachés aux cellules épithéliales squameuses. (C) Lavage bronchoalvéolaire coloré par FISH d’un enfant atteint de PBB montrant un biofilm de cellules épithéliales squameuses (SEC) contenant de petits groupes de Moraxella catarrhalis (flèches rouges) et d’autres bactéries non identifiées (sonde eubactérienne en jaune) associées à l’ADN de l’hôte (bleu). Le cercle indique la cellule épithéliale squameuse associée. Aucune hybridation non spécifique (sonde NONEUB en vert) n’a été observée. (D) Lavage broncho-alvéolaire coloré par FISH d’un enfant atteint de bronchectasie montrant un biofilm SEC positif pour Streptococcus pneumoniae (flèche verte) et d’autres bactéries non identifiées (sonde eubactérienne en jaune) associées à l’ADN de l’hôte (bleu). Le cercle indique la cellule épithéliale squameuse associée. Crédit : The Lancet Microbe, DOI : 10.1016/S2666-5247(21)00300-1
Une nouvelle recherche a permis de faire une percée dans la compréhension d’un facteur important des infections thoraciques récurrentes chez les enfants.
De nombreux enfants présentent une toux humide prolongée après une toux aiguë et peuvent développer une affection appelée bronchite bactérienne prolongée ou PBB. Dans une étude collaborative publiée dans le prestigieux ;” data-gt-translate-attributes=”[{” attribute=””>The Lancet Microbe journal, researchers from Menzies School of Health Research (Menzies), The Telethon Kids Institute and the University of Western Australia (UWA) used a powerful microscope to discover that some of the kids with persistent wet coughs had a bacterial slime – called a biofilm – in their lungs.
Lead author, Menzies Senior Research Fellow, Dr. Robyn Marsh says children with recurrent PBB are at increased risk of progressing to a severe lung disease called bronchiectasis.
“We know that for most kids with PBB, their cough will get better after they have had a two-week course of antibiotics, but we also know that some kids will have repeated episodes of bronchitis that never seem to get better,” Dr. Marsh said.
“This puts them at risk of developing a severe lung disease called bronchiectasis. We know that chest infections can lead to PBB and bronchiectasis, but the reasons why only some kids respond to antibiotics isn’t always clear.”
The research team used a process known as bronchoalveolar lavage (BAL) to collect a sample from the lungs for testing. During the procedure, a sterile solution is used to flush the child’s airways and capture a fluid sample containing the germs that cause the child’s chest infection. This is the first known study to demonstrate a prevalence of biofilm in affected children.
Study co-author Dr. Ruth Thornton a Research Fellow, UWA Centre for Child Health Research (affiliated with the Telethon Kids Institute) says using the powerful microscope with contrasting colors assisted in locating and identifying the bacterial slime which is present in the affected lungs.
“This is an important discovery as we know that when bacteria live in these slimes they can be more than a thousand times more resistant to antibiotics than the bacteria that cause the acute infections that you take your child to the doctor for. This means that when you stop antibiotics your child is likely to get yet another infection,” Dr. Thornton said.
Professor Anne Chang AM, Menzies Head of Child Health described the study results as an exciting way forward to help treat the children who have been suffering.
“This is really exciting. We’ve suspected these children have biofilm-associated infections for a while but until now, no one has proven it. Now that we’ve seen it, we can start investigating new ways to treat these children so that fewer of them will progress to having severe lung disease,” Prof Chang said.
Reference: “Prevalence and subtyping of biofilms present in bronchoalveolar lavage from children with protracted bacterial bronchitis or non-cystic fibrosis bronchiectasis: a cross-sectional study” by Robyn L Marsh, PhD; Michael J Binks, PhD; Heidi C Smith-Vaughan, PhD; Maxine Janka, BSc; Sharon Clark, BBioMedSc; Prof Peter Richmond, MD; Prof Anne B Chang, PhD and Ruth B Thornton, PhD, 1 February 2022, The Lancet Microbe.
DOI: 10.1016/S2666-5247(21)00300-1
Menzies School of Health Research
Menzies is one of Australia’s leading medical research institutes dedicated to improving the health and wellbeing of Aboriginal and Torres Strait Islanders, and a leader in global and tropical research into life-threatening illnesses, Menzies continues to translate research into effective partnerships and programs in communities across Australia and the Asia-Pacific region.